The alarm blares, the coffee brews, and a new shift dawns. As nurses, we walk into a world of controlled chaos, where every second counts, and every detail matters. We carry the weight of lives in our hands, and with that comes the immense responsibility of accurate assessment, timely intervention, and seamless communication. But let's be honest, sometimes it feels like we're juggling flaming chainsaws while riding a unicycle – exhilarating, yes, but also utterly terrifying without the right tools.
I remember my early days on the floor, fresh out of nursing school, armed with a textbook knowledge that suddenly felt woefully inadequate. My preceptor, a battle-hardened veteran with eyes that saw everything, would rattle off patient details during handoff at what felt like warp speed. I’d scribble furiously on any scrap of paper I could find – a torn piece of a medication label, the back of an old order sheet, even my own hand once! I’d leave handoff feeling more confused than enlightened, my notes a cryptic mess only I (sometimes) understood. The anxiety of forgetting a crucial detail, missing a subtle change, or giving a disjointed report was palpable. It wasn’t just about my performance; it was about patient safety, about delivering the best care possible. That’s when I discovered the magic, the sheer relief, of a well-designed printable nursing report sheet. It wasn't just paper; it was a lifeline, a silent partner in the demanding rhythm of nursing. It transformed my shifts, not just organizing my thoughts, but giving me a confidence I desperately needed.
This isn't just about finding a piece of paper. It's about finding *your* piece of paper – the one that empowers you to be the best nurse you can be. It's about streamlining your workflow, sharpening your critical thinking, and ensuring every patient gets the meticulous care they deserve. Whether you're a nursing student grappling with your first clinical, a new graduate navigating the complexities of independent practice, or a seasoned veteran looking for a fresh approach to organization, this comprehensive guide is for you. We're going to dive deep, exploring everything from the foundational "why" behind these sheets to advanced customization techniques, specialty-specific templates, and even the subtle art of using them for impeccable handoffs. Trust me, by the end of this, you’ll not only understand the power of a great report sheet but you’ll be equipped to choose, create, and utilize one that truly fits your unique nursing journey.
---
### Table of Contents
- [The Unsung Hero: Why Printable Nursing Report Sheets Are Non-Negotiable](#the-unsung-hero-why-printable-nursing-report-sheets-are-non-negotiable)
- [Anatomy of Excellence: Essential Elements of a Top-Tier Report Sheet](#anatomy-of-excellence-essential-elements-of-a-top-tier-report-sheet)
- [Tailored to Your Turf: Specialty-Specific Printable Nursing Report Sheets](#tailored-to-your-turf-specialty-specific-printable-nursing-report-sheets)
- [DIY vs. Download: Crafting Your Own or Finding the Perfect Template](#diy-vs-download-crafting-your-own-or-finding-the-perfect-template)
- [The Art of the Handoff: Using Your Report Sheet for Seamless Transitions](#the-art-of-the-handoff-using-your-report-sheet-for-seamless-transitions)
- [Beyond the Paper: Integrating Digital Tools and Advanced Strategies](#beyond-the-paper-integrating-digital-tools-and-advanced-strategies)
- [From Student to Seasoned Pro: Report Sheets for Every Career Stage](#from-student-to-seasoned-pro-report-sheets-for-every-career-stage)
- [Legal Eagle & Ethical Compass: Documentation Best Practices with Your Sheet](#legal-eagle--ethical-compass-documentation-best-practices-with-your-sheet)
- [How to Choose the Best Printable Nursing Report Sheet for Your Needs](#how-to-choose-the-best-printable-nursing-report-sheet-for-your-needs)
- [Common Pitfalls to Avoid with Nursing Report Sheets](#common-pitfalls-to-avoid-with-nursing-report-sheets)
- [Advanced Tips for Seasoned Nurses: Elevating Your Report Sheet Game](#advanced-tips-for-seasoned-nurses-elevating-your-report-sheet-game)
- [Conclusion: Empower Your Practice, One Sheet at a Time](#conclusion-empower-your-practice-one-sheet-at-a-time)
---
The Unsung Hero: Why Printable Nursing Report Sheets Are Non-Negotiable
Let's face it, nursing is a profession built on precision, critical thinking, and the ability to pivot at a moment's notice. In the whirlwind of a shift, where alarms chime, call lights flash, and patient needs are constantly evolving, how do we keep all the crucial pieces of information straight? The answer, my friends, often lies in the humble yet mighty printable nursing report sheet. It’s not just a piece of paper; it’s a strategic tool that underpins everything we do, from basic care to life-saving interventions.
Here’s why these sheets are absolutely essential for every nurse:
1. Enhances Patient Safety: This is paramount. A well-organized report sheet acts as a cognitive aid, ensuring you don't miss vital signs, medication timings, assessment findings, or critical orders. When I was a new grad, I once almost forgot to check a stat potassium level because it was buried in a messy note. Thankfully, a quick glance at my nascent (and still messy) report sheet jogged my memory. It literally could have made a difference.
2. Streamlines Information Retrieval: Imagine a patient suddenly decompensates, and you need their last blood pressure, current neuro status, and recent pain medication history *now*. Fumbling through charts or trying to recall from memory wastes precious seconds. A good report sheet puts all this at your fingertips.
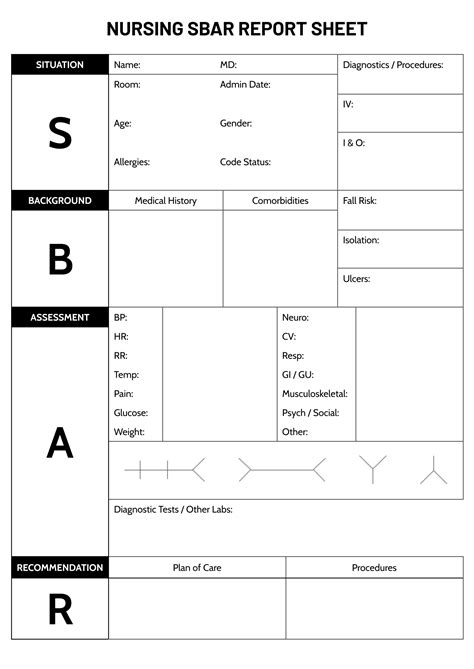
3. Facilitates Effective Handoff: The SBAR (Situation, Background, Assessment, Recommendation) framework is a gold standard for handoff, and a structured report sheet naturally guides you through this process. It ensures a comprehensive, concise, and consistent report, reducing the risk of communication errors. My preceptor, for all her speed, always had an immaculate report sheet. She'd glide through handoff, touching on every key point, and it was her sheet that made it possible.
4. Boosts Critical Thinking: When you consistently record and review patient data on a structured sheet, you start to see patterns, anticipate potential problems, and connect the dots. It trains your brain to think systematically, moving beyond just collecting data to *interpreting* it.
5. Reduces Stress and Anxiety: For new nurses especially, the sheer volume of information can be overwhelming. A report sheet provides a sense of control and reduces the fear of forgetting something important. It's like having a safety net. I definitely felt this relief when I finally found a sheet that clicked with my brain.
6. Aids in Accurate Documentation: While your report sheet isn't typically part of the legal medical record, it's an invaluable tool for ensuring your official charting is complete and accurate. You can cross-reference your notes before documenting, minimizing errors and omissions.
7. Supports Time Management: By having a clear overview of your patient load, scheduled tasks (meds, treatments), and upcoming events (tests, discharges), you can better prioritize and manage your time throughout the shift, leading to a more efficient workflow.
8. Personalized Workflow: Unlike standardized electronic health records (EHRs), a printable sheet can be customized to *your* preferred flow, *your* way of thinking, and *your* specific unit's needs. This personalization is key to making it truly effective.
9. Learning Tool for Students: For nursing students, a report sheet is indispensable. It helps them organize their clinical day, remember to perform all necessary assessments, and prepare for post-conference discussions. It's like a mini-checklist for becoming a competent nurse.
10. Prepares for Unexpected Events: When things go sideways – a rapid response, a code – having all your patient's baseline information and recent events neatly organized can be a lifesaver. You can quickly provide a concise report to the medical team without scrambling.
11. Reflects Professionalism: A nurse who is organized and provides a clear, comprehensive report at handoff projects an image of competence and professionalism. Your report sheet contributes significantly to this.
12. Adapts to Tech Failures: In an age of increasing reliance on EHRs, a physical report sheet provides a crucial backup in case of system downtime or technical glitches. You can still provide safe, informed care even when the computers are down. This is something I've personally experienced during a major system outage – my paper sheet was a lifesaver!
Anatomy of Excellence: Essential Elements of a Top-Tier Report Sheet
So, what makes a printable nursing report sheet truly effective? It's not just about having lines and boxes; it's about strategic design that anticipates your needs and guides your thought process. Think of it as your personal cockpit dashboard, displaying all the critical indicators at a glance.
Here are the essential elements you should look for or include when designing your ideal sheet:
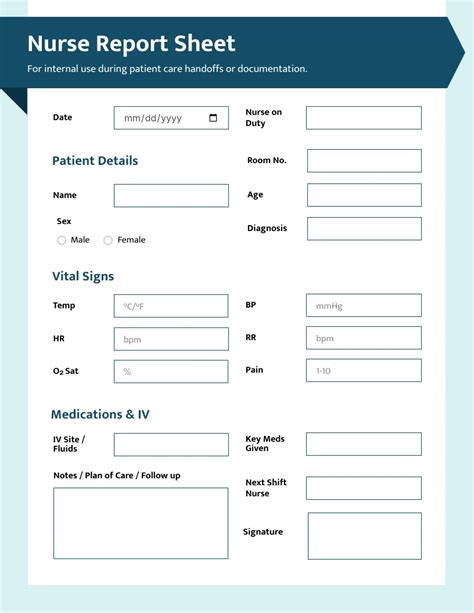
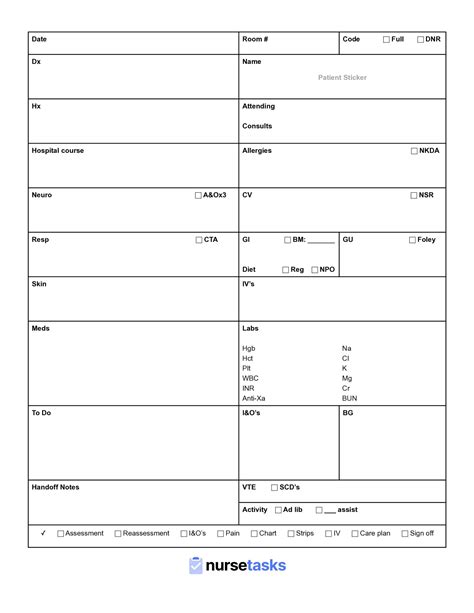
1. Patient Demographics & Basic Information:
- Room Number: Crucial for quick location.
- Patient Name: Obvious, but essential.
- Age/DOB: Helps with age-specific considerations and identity verification.
- Diagnosis (Primary & Secondary): Provides context for care.
- Code Status: (e.g., Full Code, DNR, DNI) – Absolutely non-negotiable and usually highlighted. *I always put this in bold red on my sheets.*
- Allergies: Another non-negotiable that should be prominently displayed.
- Attending Physician/Team: Knowing who to call is vital.
2. Shift-Specific To-Dos & Priorities:
- Time Block/Hourly Schedule: A column or section to jot down tasks by time (e.g., 0800 meds, 0900 dressing change, 1000 PT). This is a game-changer for time management.
- "Must-Dos" / Critical Tasks: A dedicated space for high-priority items like stat labs, consults to page, or specific assessments.
- Goals for the Shift: What are you hoping to achieve for this patient today? (e.g., ambulate x2, pain control, discharge teaching).
3. Comprehensive Assessment Checklist (Head-to-Toe):
- Neuro: LOC, orientation, pupils, strength, sensation, pain scale (location, quality, intensity). *My go-to here is a quick "A&O x4, PERRLA, strength equal" checkbox.*
- Cardiac: Heart sounds, rhythm, edema, capillary refill, pulses (location, quality).
- Respiratory: Breath sounds, oxygen requirements, cough, sputum, respiratory effort.
- GI: Diet, bowel sounds, last BM, abdominal assessment, N/V.
- GU: Urine output (Foley?), color, clarity, frequency.
- Skin: Color, temperature, turgor, integrity, wounds/incisions (location, size, drainage).
- IV Access: Site, type, date, fluids infusing.
- Pain Assessment: Often integrated into neuro, but a separate section can be useful for trends.
4. Vital Signs & Trends:
- Hourly/Timed Slots: Spaces to record BP, HR, RR, Temp, SpO2. This helps you quickly spot trends.
- Pain Score: Often recorded with vitals.
5. Medication Administration Record (MAR) Snapshot:
- Scheduled Meds: A condensed list of key medications, especially time-critical ones (insulins, antibiotics, PRN effectiveness). I usually jot down the time, med name, and dose, then check it off as given.
- PRN Meds Administered: Space to note what PRN was given, when, and its effectiveness.
6. Labs & Diagnostics:
- Pending Labs: What's ordered and when is it due?
- Results (Key Values): Space for critical lab results (e.g., Hgb, electrolytes, INR, cultures). I often draw a small "up" or "down" arrow next to abnormal values to quickly show trends.
- Imaging/Consults: Any scheduled or pending tests (e.g., X-ray, CT, MRI, cardiology consult).
7. Intake and Output (I&O):
- Hourly/Shift Totals: Space to track IV fluids, oral intake, urine output, drains, emesis.
- Fluid Balance: A simple running total or a place to calculate it.
8. Lines, Tubes, Drains (LTD):
- Specifics: Central lines, peripheral IVs, foleys, NGs, chest tubes, surgical drains – their location, size, and insertion date. This is where you track potential infection risks.
9. Plan of Care / Goals:
- Short-Term Goals: What do you want to achieve *this shift*?
- Long-Term Goals: What is the overall plan for the patient (e.g., discharge planning, new medications, therapy)?
- Interventions: What actions are you taking to meet these goals?
10. "Other" / Important Notes / Communication:
- Family Communication: Who did you speak to, what was discussed?
- Physician Communication: When did you call the doctor, what was the update/order?
- Interdisciplinary Team: PT/OT/SW updates.
- Mental Health/Psychosocial: Any relevant observations.
- Discharge Planning: Key teaching points, equipment needs.
- Any "Red Flags" or Concerns: A quick space to note anything that worries you or needs closer monitoring.
11. Handoff Section:
- SBAR-friendly areas: Spaces that naturally guide you to fill in Situation, Background, Assessment, and Recommendation points for your oncoming colleague.
My subjective take: For me, the most undervalued section is often the "Goals for the Shift" and "Pending Tasks" area. I thrive on checklists, and having a clear, visual representation of what needs to get done, and what the overall aim is for the patient's day, significantly reduces my anxiety and improves my efficiency. It helps me prioritize when everything feels urgent.
Tailored to Your Turf: Specialty-Specific Printable Nursing Report Sheets
One size rarely fits all, and this is especially true for printable nursing report sheets. What works perfectly for a medical-surgical nurse might be completely inadequate for an ICU nurse or a labor & delivery nurse. The beauty of these sheets is their adaptability. Let's explore how different specialties can customize their sheets to meet their unique demands.
1. Medical-Surgical (Med-Surg) Nursing Report Sheet:
- Focus: Broad systems assessment, medication management for multiple patients (often 4-6), discharge planning, wound care.
- Key Elements:
- Multi-patient layout: Often 2-4 patients per page.
- Detailed I&O: Crucial for fluid balance management.
- Comprehensive assessment checklist: Covering all body systems.
- Post-op status section: For surgical patients (e.g., drains, incisional pain, ambulation status).
- Discharge Planning Notes: Space for patient education topics, follow-up appointments.
- Hypothetical Scenario: *I once had a Med-Surg sheet that had a dedicated section for "Social Determinants of Health." It prompted me to ask about housing and food security, which was critical for a patient with frequent readmissions due to uncontrolled diabetes.* This sheet changed how I approached discharge planning.
2. Intensive Care Unit (ICU) Nursing Report Sheet:
- Focus: Hemodynamic stability, advanced monitoring, titration of critical drips, frequent neuro checks, ventilator management, complex lab interpretation.
- Key Elements:
- Hourly Vital Signs & Titratable Drips: Dedicated, large sections for frequent recordings and adjustments.
- Neurological Assessment (e.g., GCS, RASS, pupil checks): Often hourly or even more frequently.
- Ventilator Settings: Mode, FiO2, PEEP, tidal volume, pressures.
- Hemodynamic Monitoring: CVP, arterial lines, PA catheters.
- Sedation/Analgesia Assessment: RASS scores, pain scores.
- Renal Replacement Therapy (CRRT/Dialysis): Settings and output.
- Detailed Lines, Tubes, Drains (LTD): Central lines, arterial lines, foley, NGT, chest tubes, etc., with insertion dates and assessment notes.
- Hypothetical Scenario: *Working in the ICU, I customized my report sheet to include a dedicated "trending" section for lactate levels and vasopressor doses. This visual aid helped me anticipate changes in patient status much faster than just looking at individual numbers in the EHR.*
3. Emergency Department (ED) Nursing Report Sheet:
- Focus: Rapid assessment, triage, quick turnaround, managing multiple patients with varying acuities, concise documentation for disposition.
- Key Elements:
- Triage Information: Chief complaint, arrival time, ESI level.
- Quick "Snapshot" Assessment: ABCs, brief neuro, pain.
- Trauma Scores (if applicable): GCS, mechanism of injury.
- Lab/Imaging Status: Clear sections for pending, resulted, and critical values.
- Medication Administration: Focus on stat meds, pain control, antibiotics.
- Disposition Planning: Admitted, discharged, transferred.
- Compact design: Often one patient per page, designed for speed.
- My subjective take: An ED sheet needs to be like a mental flowchart in paper form. My favorite ones have bolded sections for "Red Flags" or "Immediate Interventions" to ensure nothing is missed in the organized chaos.
4. Labor & Delivery (L&D) Nursing Report Sheet:
- Focus: Maternal and fetal monitoring, labor progression, pain management, post-partum care, newborn assessment.
- Key Elements:
- Maternal Status: G/P, EDC, current gestation, OB history, pertinent medical history.
- Fetal Monitoring: FHR baseline, variability, accelerations/decelerations, contractions (frequency, duration, intensity).
- Labor Progression: Cervical dilation, effacement, station, membrane status.
- Pain Management: Epidural details, last pain med, effectiveness.
- Post-Partum: Fundus, lochia, perineum, breast/bottle feeding.
- Newborn Assessment: APGARs, vital signs, feeding, void/stool.
- Hypothetical Scenario: *I saw an L&D nurse who had a dedicated section for "partner involvement." It prompted her to ask about the partner's comfort level and educational needs, which really enhanced the family-centered care she provided.*
5. Pediatric Nursing Report Sheet:
- Focus: Age-appropriate assessments, growth & development, parental involvement, fluid balance, medication calculations (weight-based).
- Key Elements:
- Weight (kg) & BSA: Crucial for medication dosing.
- Age-Specific Vitals: Normal ranges change dramatically by age.
- Developmental Milestones: Space to note observations.
- Parent/Guardian Information: Contact, involvement level.
- Nutrition: Feeding method, intake, output.
- Immunization Status: Important for infection control.
- IV Access: Smaller gauges, specific sites.
- My favorite thing about peds sheets: They often have a small section for "comfort items" or "distraction techniques" – a small but powerful reminder of the unique needs of children.
6. Telemetry/Cardiac Nursing Report Sheet:
- Focus: Cardiac rhythm interpretation, EKG changes, cardiac medications, signs of cardiac compromise, peripheral vascular assessment.
- Key Elements:
- Cardiac Rhythm Strip interpretation: Space to note rhythm, rate, PR, QRS, QT intervals.
- EKG Changes: Stemi, NSTEMI, ischemia.
- Cardiac Medications: Antiarrhythmics, anticoagulants, antihypertensives.
- Peripheral Pulses & Edema: Detailed assessment.
- Chest Pain Assessment: PQRST.
- Cardiac History: MIs, CHF, bypass surgery.
7. Post-Anesthesia Care Unit (PACU) Nursing Report Sheet:
- Focus: Post-op recovery, airway management, pain control, nausea/vomiting, immediate surgical site assessment, discharge criteria.
- Key Elements:
- Pre-op Hx (brief): Key allergies, past medical.
- Anesthesia Report: Type of anesthesia, meds given, EBL.
- Frequent Vitals: Often every 5-15 minutes.
- Pain & Nausea Scores: With space for interventions and effectiveness.
- Surgical Site Assessment: Dressing, drainage.
- Aldrete Score/Discharge Criteria: Clear checklist for discharge from PACU.
8. Rehabilitation Nursing Report Sheet:
- Focus: Functional assessment, mobility, bowel/bladder training, therapy goals, patient education for self-care.
- Key Elements:
- Functional Status: ADLs, mobility (ambulation, transfers).
- Therapy Goals & Progress: PT, OT, SLP notes.
- Bowel/Bladder Program: Schedule, outcomes.
- Patient/Family Education: What was taught, what needs to be reinforced.
- Discharge Planning: Equipment needs, home setup.
9. Home Health/Hospice Nursing Report Sheet:
- Focus: Comprehensive assessment of home environment, caregiver support, social determinants of health, symptom management (hospice), medication reconciliation, teaching.
- Key Elements:
- Home Environment Safety: Falls risk, resources.
- Caregiver Assessment: Capacity, needs, education.
- Social Support: Family, community.
- Symptom Management: Pain, dyspnea, nausea (hospice).
- Medication Reconciliation: Detailed list, adherence.
- Teaching Provided: Specifics for patient/family.
- Goals of Care: Patient/family wishes.
10. Mental Health Nursing Report Sheet:
- Focus: Mental status assessment, safety planning, behavioral observations, medication adherence, therapeutic communication, group participation.
- Key Elements:
- Mental Status Exam: Appearance, mood, affect, thought process, content, perception, insight, judgment.
- Safety Assessment: Suicide/homicide ideation, elopement risk.
- Behavioral Observations: Agitation, withdrawal, social interaction.
- Medication Adherence: Especially for psychotropic meds.
- Group Therapy Participation: Attendance, engagement.
- Coping Strategies: What works for the patient.
11. Oncology Nursing Report Sheet:
- Focus: Chemotherapy protocols, symptom management (nausea, fatigue, mucositis), neutropenic precautions, central line care, psychosocial support.
- Key Elements:
- Chemotherapy Regimen: Drugs, cycles, side effects.
- Neutropenic Precautions: Monitoring for infection.
- Central Line Care: Assessment, dressing changes.
- Symptom Management: Nausea, pain, fatigue, anxiety.
- Blood Product Administration: Transfusion details.
- Psychosocial Support: Anxiety, depression, family coping.
12. Outpatient/Clinic Nursing Report Sheet:
- Focus: Appointment scheduling, patient education, medication refills, follow-up calls, brief assessments for specific complaints.
- Key Elements:
- Appointment Details: Time, reason for visit.
- Focused Assessment: Relevant to chief complaint.
- Medication Reconciliation: Current meds, changes.
- Education Provided: Handouts, verbal instructions.
- Follow-up Plan: Next appointment, referrals.
- Call Log: Documenting patient calls.
The key takeaway here is that your printable nursing report sheet isn't static. It's a living document that should evolve with your practice and your environment. Take inspiration from these examples, but never hesitate to tweak them to perfectly fit *your* specific needs.
DIY vs. Download: Crafting Your Own or Finding the Perfect Template
The quest for the perfect printable nursing report sheet often leads down two paths: designing your own from scratch or finding a pre-made template to download. Both have their merits, and the "best" approach often depends on your personal preferences, technical skills, and how much time you have.
### The DIY Approach: Building Your Own Masterpiece
Creating your own report sheet can be incredibly empowering. It ensures every single element is exactly where you want it and perfectly tailored to your workflow.
Pros of DIY:
- Ultimate Customization: Every box, every line, every heading is exactly what *you* need.
- Reflects Your Workflow: You can arrange information in a way that aligns with your thought process during a shift.
- Deeper Understanding: The process of designing forces you to think critically about what information is essential and why.
- Evolves with You: Easy to tweak and update as your practice changes or you move to a new unit.
Cons of DIY:
- Time-Consuming: Requires significant time and effort initially.
- Design Skills: Might be frustrating if you're not comfortable with word processors or design software.
- Trial and Error: Expect to revise it several times before it's perfect.
How to DIY Your Report Sheet:
1. Brainstorm Your Needs:
- What unit do you work on? (Med-Surg, ICU, ED, etc.)
- How many patients do you typically have?
- What are the absolute *must-have* pieces of information for each patient?
- What order do you typically perform your assessments/tasks?
- What information do you *always* forget or have to look up? (e.g., specific lab ranges, common medication doses).
2. Choose Your Tool:
- Microsoft Word/Google Docs: Excellent for basic layouts, tables, columns, and text. Most accessible.
- Microsoft Excel/Google Sheets: Great for creating structured grids, especially if you want to track trends or calculations.
- Canva/Adobe InDesign: For more graphically appealing, professional-looking designs, but steeper learning curve.
- Pen and Paper (initial sketch): Don't underestimate the power of sketching it out first!
3. Start with the Basics:
- Begin with patient demographics, code status, and allergies.
- Create sections for vital signs, assessment categories (Neuro, Cardiac, Resp, etc.), I&O, meds, and labs.
- Think about flow: Do you want a horizontal layout (patient names across the top, categories down the side) or vertical (each patient gets a full column)?
4. Add Your Personal Touches:
- Include a "To-Do" checklist for the shift.
- A section for "Questions for MD/Team."
- Space for discharge planning notes.
- A small area for "Red Flags" or "Important Reminders."
5. Test and Refine:
- Print a few copies and use them during your shifts.
- After each shift, review what worked well and what didn't. Did you have enough space? Was the information easy to find? Did you miss anything crucial?
- Don't be afraid to iterate! My first DIY sheet was a disaster, but after three revisions, it became my most reliable companion. *I remember one shift where I realized I'd forgotten to add a "last BM" section, leading to a frantic search through the EHR. That night, it was the first thing I added