When moments matter most, clarity and accuracy are non-negotiable. If you've ever found yourself in a high-stakes medical situation, whether in a bustling emergency room, a quiet clinic, or even just as a concerned first responder, you know the immense pressure of quick, reliable assessment. That’s where the Glasgow Coma Scale (GCS) comes in—a universal language for evaluating a patient's level of consciousness.
I've been there, trying to quickly recall the precise scoring criteria under pressure, wishing I had a tangible, quick-reference guide right at my fingertips. Trust me, you don’t want to mess this up! Having a printable Glasgow Coma Scale isn't just convenient; it's a critical tool that ensures consistency, minimizes errors, and empowers you to make informed decisions when every second counts. It's about empowering healthcare professionals, students, and even concerned caregivers with a reliable way to monitor neurological status.
---
GCS Explained: The Foundation of Neurological Assessment
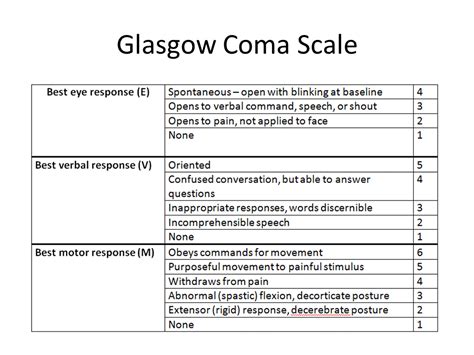
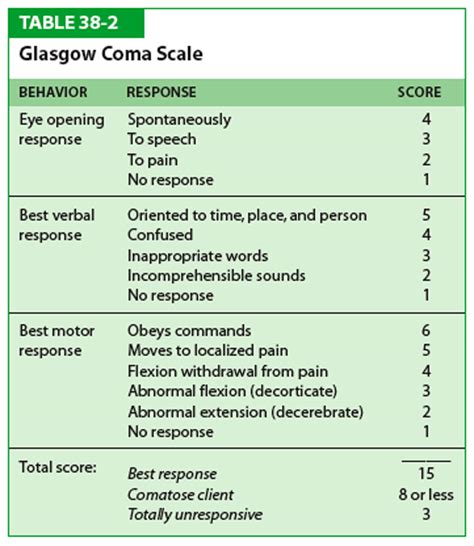
Understanding the Glasgow Coma Scale is the first critical step. It’s a standardized tool designed to objectively assess the level of consciousness in patients, primarily those with suspected brain injury. Developed in 1974, it measures three components: Eye Opening, Verbal Response, and Motor Response, each with a specific scoring range. A perfect score is 15, indicating full consciousness, while a score of 3 is the lowest possible, often associated with severe neurological impairment.
- Eye Opening (E: 1-4):
- 4: Spontaneous
- 3: To speech
- 2: To pain
- 1: No response
- Verbal Response (V: 1-5):
- 5: Orientated
- 4: Confused conversation
- 3: Inappropriate words
- 2: Incomprehensible sounds
- 1: No response
- Motor Response (M: 1-6):
- 6: Obeys commands
- 5: Localizes to pain
- 4: Withdraws from pain
- 3: Flexion to pain (decorticate)
- 2: Extension to pain (decerebrate)
- 1: No response
My insight: When I was learning this, a senior nurse told me, "Think of it as looking at the brain's 'volume dial' for how it responds to the world." This simple analogy helped me grasp the concept more quickly.
Why a Printable GCS is Your Go-To Tool
In the fast-paced world of emergency medicine and critical care, relying solely on memory can be risky. A printable Glasgow Coma Scale sheet serves as an invaluable aide-mémoire and a tangible record-keeping tool. It offers immediate access to the scoring criteria, ensuring you don't miss any nuances, especially when dealing with complex patient presentations or during a stressful shift.
- Instant Reference: No need to search on your phone or flip through a textbook.
- Consistency: Helps maintain uniformity in assessments across different shifts or care providers.
- Documentation Aid: Many printable versions include space for date, time, and sequential scores, crucial for tracking trends.
- Training Tool: Perfect for medical students, new nurses, or first responders practicing their assessment skills.
- Offline Accessibility: Essential in situations where internet access is limited or unreliable.
Scenario: I once saw a junior doctor hesitate during a trauma assessment, trying to recall the exact motor response scoring. Having a compact, printable Glasgow Coma Scale card pulled from their pocket immediately resolved the uncertainty, allowing for a swift and accurate assessment that directly informed the patient's immediate care.
Mastering the Score: A Step-by-Step Guide to Assessment
Using a printable Glasgow Coma Scale effectively goes beyond just having the sheet; it's about applying it systematically. This structured approach helps ensure accuracy and reduces the chance of overlooking critical signs.
1. Assess Eye Opening: Start by observing if the patient opens their eyes spontaneously. If not, try speaking to them. If still no response, apply a noxious stimulus (e.g., sternal rub, trapezius squeeze).
- *Example:* If a patient opens their eyes only when you speak their name clearly, their Eye Opening score is 3.
2. Evaluate Verbal Response: Ask the patient simple questions like "What is your name?" or "Where are you?" Listen carefully to their answers.
- *Example:* A patient who can tell you their name and location accurately scores a 5 for Verbal Response. If they just utter random, unrelated words, that's a 3.
3. Determine Motor Response: Give the patient a command, such as "Squeeze my hand" or "Lift your arm." If they don't respond, apply a painful stimulus to assess their motor reaction.
- *Example:* If a patient immediately pulls their hand away when you apply pain to their nail bed, their Motor Response is 4 (withdraws from pain).
4. Total the Scores: Add the individual scores for Eye, Verbal, and Motor responses to get the total GCS score.
- *Example:* E4 + V5 + M6 = GCS 15.
5. Document Immediately: Write down the individual scores (EVM) and the total GCS on your printable sheet, noting the date and time.
My observation: Many times, I've seen individuals rush the assessment, especially the verbal or motor components. The beauty of a structured, printable Glasgow Coma Scale is that it encourages you to go through each step deliberately, even under pressure.
Navigating Nuances: Special Considerations & Common Pitfalls
While the GCS is a robust tool, its accurate application requires an understanding of specific situations and potential misinterpretations. This is where your expertise truly shines.
- Intubated Patients: If a patient is intubated, their Verbal Response cannot be assessed. This is denoted by "Vt" (Verbal intubated). Their GCS score will then be E + M + Vt (e.g., GCS E4M6Vt).
- Sedated Patients: Sedation directly affects consciousness. Note this clearly in your documentation. A GCS score in a sedated patient reflects their response *under sedation*, not necessarily their baseline neurological status.
- Language Barriers or Deafness: These can affect verbal response. Ensure you differentiate between true impaired consciousness and communication barriers.
- Pre-existing Conditions: Assess against baseline if known. Conditions like pre-existing paralysis can impact motor response.
- Common Pitfall: Not Applying Adequate Pain: To elicit a response to pain, the stimulus must be sufficient. A gentle rub won't do; use a sternal rub, trapezius squeeze, or nail bed pressure.
- Common Pitfall: Misinterpreting Decorticate/Decerebrate Posturing: These are specific, abnormal motor responses indicating significant brain injury. Decorticate (flexion) is typically better than Decerebrate (extension).
- *Warning:* Don't be like me when I first started and confuse these; precise identification is crucial for prognosis and treatment!
Subjective Tip: I find that practicing the GCS on a mannequin or even a cooperative colleague (pretending to be unresponsive) helps to build muscle memory for the physical assessment components before facing a real-life critical situation.
Beyond the Numbers: Interpreting GCS Changes & Documentation

The power of the Glasgow Coma Scale isn't just in the initial score; it's in tracking changes over time. A seemingly small drop in GCS, even one point, can indicate significant neurological deterioration requiring urgent intervention.
- Trend Monitoring: Regular, sequential GCS assessments are vital. A deteriorating trend is a major red flag, even if the absolute score still seems "high."
- *Example:* A patient initially GCS 14 (E4V5M5) who later becomes GCS 12 (E3V4M5) is a serious concern, despite still being "awake."
- Communication: Clearly communicate GCS scores and any changes to the healthcare team. Use the full E+V+M breakdown for clarity (e.g., "GCS 10, E3V3M4, down from GCS 12 an hour ago"). This detailed communication is far more valuable than just saying "GCS 10."
- Clinical Context: Always interpret the GCS score within the full clinical picture. A GCS of 8 might be concerning for a head injury patient but expected for someone deeply sedated.
- Documentation is Key: Beyond the score, document the *reason* for the patient's GCS. "Patient sedated" or "Patient intubated" provides crucial context. Also note specific observations like pupil size and reactivity, which complement the GCS.
My takeaway: What I've learned the hard way is that relying on someone else's assessment without doing your own, especially when you see a trend change, is a mistake. Always re-assess yourself and trust your findings, documenting them clearly on your printable Glasgow Coma Scale sheet.
Choosing Your Print: Different Formats and Where to Find Them

The "printable" aspect of the printable Glasgow Coma Scale is about convenience and accessibility. There are various formats available, catering to different needs.
- Pocket Cards: Small, laminated cards perfect for clipping onto an ID badge or keeping in a scrub pocket. These often include pupil assessment charts as well.
- Full-Page Checklists: Larger printouts, ideal for charting at the bedside or for training sessions. These usually have ample space for multiple time-stamped assessments.
- Digital Templates (for printing): Many medical websites and educational resources offer free PDF downloads. Search for "GCS chart PDF" or "neurological assessment form printable."
- Customizable Versions: Some templates allow you to add your hospital's logo or specific departmental instructions before printing.
Practical Tip: I personally prefer a laminated pocket-sized printable Glasgow Coma Scale card. It’s durable, easy to clean, and always available—a non-negotiable part of my clinical toolkit.
---
The Glasgow Coma Scale is more than just a set of numbers; it's a vital communication tool in emergency and critical care settings. Having a printable Glasgow Coma Scale on hand empowers you to perform accurate, consistent assessments, ensuring that every patient receives the precise care they need. Now, go forth and make accurate assessments—it could truly make a difference!